Are you experiencing digestive issues during pregnancy? You are not alone. Pregnancy has a big impact on your digestive system.

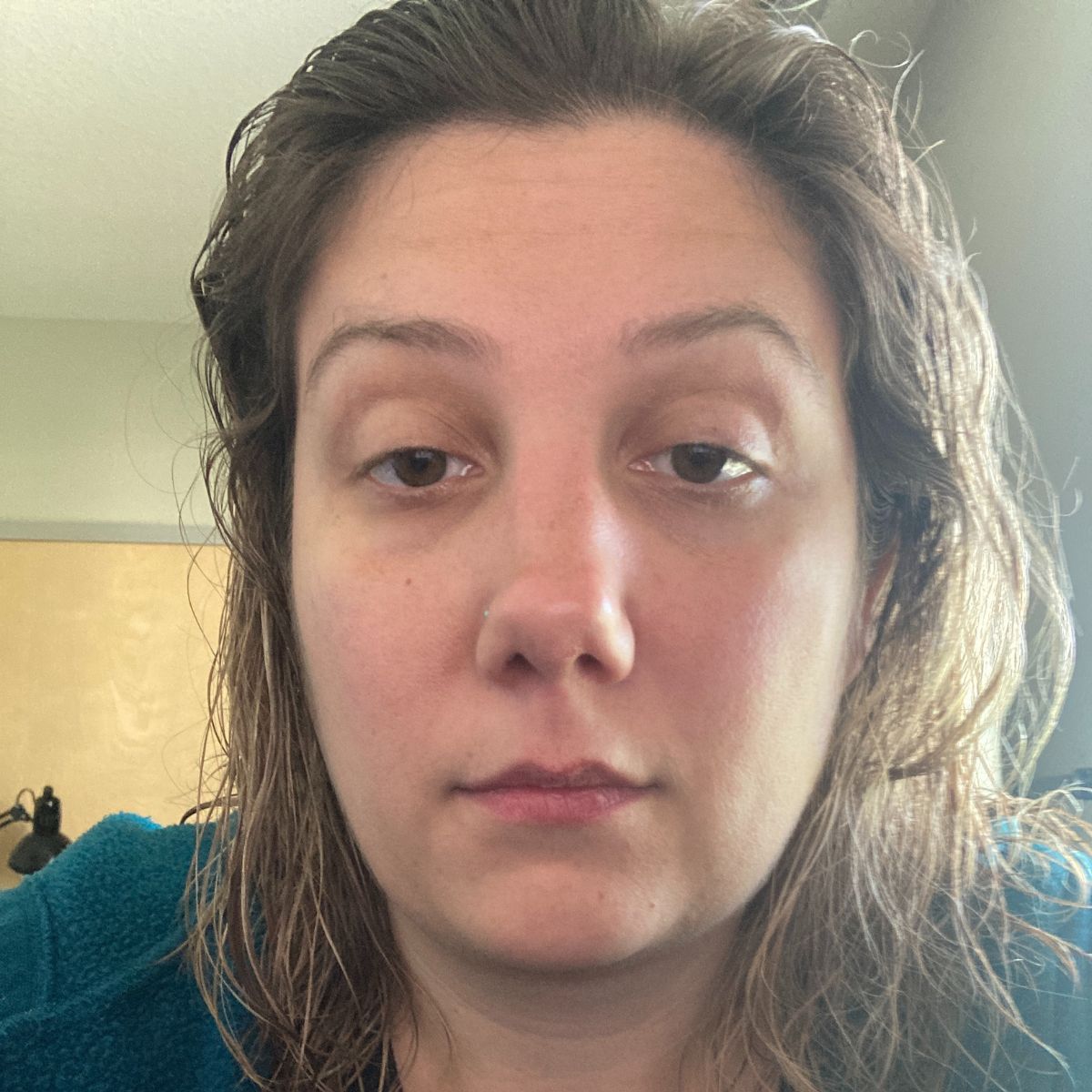
This article is a personal account of my digestive issues during pregnancy, my approach to nutrition while pregnant, and the solutions that did and did not work for me.
While I am a prenatal dietitian, remember this is not meant as medical advice. It is a personal reflection of my experience and intended for informational and educational purposes only. However, I’d love to work with you individually so check out my services here.
Table of Contents
My pregnancy journey
I was fortunate to have a healthy pregnancy with a ton of family support and love (I’m writing this at 34 weeks, so hopefully that stays true throughout my pregnancy).
I fell into the category of “advanced maternal age” because I became pregnant at 37 and delivered at 38 years old. I had many friends and cousins who already had kids so I had a good depth chart of people to seek advice from.
It was a time of excitement and general upheaval in my life.
At 17 weeks pregnant, my husband and I moved from Minneapolis back to the East Coast where we are from.
At 20 weeks pregnant, my husband and I tested positive for COVID-19.
We spent two months living with my in-laws who graciously let us stay with them in their home on Long Island. When I was around 28 weeks, we moved to an apartment in Norwalk, CT where I write this article from.

I also changed providers from my Minneapolis care team to the care team at Norwalk Hospital. I decided to work with a certified nurse midwife, rather than an OB (although they all work together) and I’m really happy I did.
Lastly, my business was in flux. I ended up securing two per diem/freelance opportunities–one for writing and another for clinical work at ~33 weeks. I also saw some gains in my business.
I was scared about how I would contribute to my family’s financial situation but also happy that I had a flexible situation and knew that we would make it work. Work was a good distraction from the aches and pains of pregnancy.
What causes digestive issues during pregnancy
Digestive issues during pregnancy occur for a few different reasons. I like to think of them as hormonal, mechanical and dietary (1).
First: hormonal. Pregnancy hormones, progesterone and relaxin, slow down digestion. The pregnancy hormones prepare your body for labor by causing your muscles and connective tissue to relax. This slows digestion and allows for maximization of nutrient absorption.
Second: mechanical. The pressure of a growing uterus also impacts digestion. The uterus and baby growing inside the uterus push on your intestines, bladder, and esophagus.
Finally: dietary. Prenatal vitamins and changes in diet also impact digestion during pregnancy.

The end result is:
- Nausea and/or vomiting (known as morning sickness)
- Gas and bloating
- Heartburn and acid reflux
- Constipation
- Diarrhea
- Frequent urination
- Changes in appetite and food aversions
How my digestive system was impacted during pregnancy
Like many pregnant people, I experienced all of the digestive problems associated with pregnancy. While I knew that all the changes happening to my body were for good reason: pregnancy hormones doing their job, I still felt miserable at times.
Taste change, decrease in appetite and food aversions
No matter how much I brushed my teeth or sucked on mints or cough drops, I still had a bitter taste in my mouth.
I think this bitter taste contributed to my aversion to foods that I previously enjoyed like leafy greens, tofu, nuts, and salmon. These foods are somewhat bitter naturally.
Smelling and seeing ground turkey or raw chicken cooking disgusted me. Brewing coffee smelled like a giant ashtray filled with cigarette butts thrust in front of my nose.
Change of taste and food aversions tended to exacerbate my morning sickness.
The bad taste in my mouth and increased food aversions (plus morning sickness) definitely decreased my appetite. Who wants to eat food when it tastes or smells bad?
Some things that helped my food aversions
Sweet-tart foods: I craved watermelon, pineapple and lemonade. I have a friend who ate a pint of blueberries a day because it helped with her morning sickness!
Setting boundaries: I was very clear with my husband about what foods I could and could not tolerate. He did the bulk of the meal planning and prep during this time.
Gave myself grace: As I mentioned before, I was worried that I was depriving my baby of nutrients. I stopped worrying when I remembered that a) I was taking a prenatal vitamin and b) pregnancy was long and I would be able to eat more nutritious foods when I was feeling better.
Morning sickness was horrible
Morning sickness, which can strike at any time of the day or night, absolutely sucks.We don’t really know what causes morning sickness but it’s believed that the surge in hormones needed to encourage growth of the placenta, causes nausea and vomiting.
Before I was pregnant and I would hear stories about morning sickness (like Kate Middleton), I would think “yup, that will be me.”
Sure enough, it hit me hard. Even brushing my teeth made me want to throw up.
I worried that I was depriving my baby of nutrients because I was not eating much and definitely not eating the nutrient dense foods I was accustomed to.
I eventually had to go to urgent care because I reached a point where I could not keep down any food. It was pretty scary. At urgent care, they took my blood and gave me an anti-nausea pill which helped immediately.
I began a regiment of vitamin B6 and Unisom. This made me sleepy but helped a little. Then, I was given anti-nausea medication called Reglan which really helped.
Preggy Pops did not work for me. I could see how they would be helpful if you have a slight case of nausea but mine was more severe.
What worked to help my morning sickness
- Listening to what my body was craving.
- Keeping saltine crackers by my bed and eating them before I got out of bed.
- Ginger ale diluted with water
- Cold compress on my face
- Allowing myself to rest as much as possible
- Eating bland foods like chicken soup with noodles and bagels with plain cream cheese
- The scent of fresh lemons and putting a slice of lemon in my water. A spritz of lemon in my ginger ale helped a little.
- I always took prenatal vitamins with food, and I paused them when I was feeling especially sick.
By the time I reached week 13-14, the morning sickness dissipated along with the bitter taste in my mouth.
Second trimester stabilization

You may have heard the second trimester called the “honeymoon phase” of pregnancy. This was true for me in terms of my energy levels.
Between weeks 13-16, I experienced:
- Dissipation of morning sickness
- Return of appetite
- Increased interest in foods I enjoyed pre-pregnancy.
Unfortunately, I traded food aversions and morning sickness for constipation and heartburn.
Constipation and pregnancy
Constipation is technically defined as not pooping for more than three days. Constipation during pregnancy is a result of slowed digestion because of the pregnancy hormones.
Your intestines are muscles and the action of the muscles help move food through your digestive system. When you are pregnant, the action of these muscles slow down (orchestrated by pregnancy hormones).
This means that stool stays in your colon longer than before you were pregnant. This increases gas and bloating and creates hard pebble-like stool. Even when you are ready to pass the stools, you don’t have the same help of muscle contraction you used to have.
You may find yourself sitting on the toilet trying to pass very hard stools without much help from your colon or rectum. It is really painful and in some cases leads to hemorrhoids.
Iron in prenatal vitamins may also increase constipation during pregnancy. Even if you are technically not constipated (3 days without a bowel movement) you may not be emptying your bowels with the same thoroughness you did before.
The lifestyle strategies that helped me combat constipation during pregnancy

Monitor fiber intake: I consumed high fiber foods like whole grains, vegetables and fruit regularly and tracked how much fiber I was getting. If you want to learn more about fiber, including how much you need, check out my Essential Guide to Plant-Based Fiber.
Increase fluid intake: pregnant or not, anytime you eat more fiber than usual, you need to increase your fluid intake. This was annoying because I was already peeing a lot but I promise you it does help. I was told to drink about 100 ounces of water per day.
Move my body everyday: this one was hard when I was feeling the pregnancy fatigue, but even a ten minute walk around the block helped me stay regular-ish.
Track my bowel movements. I kept track of when I did or did not poop in my pregnancy journal.This did not increase my regularity but it gave me data to bring to my provider, if needed.
Some people find certain foods, like dairy, to be “constipating.” For my body, it’s less about avoiding certain foods and more about adding fiber, drinking plenty of water and moving.
I highly recommend working with a registered dietitian who can help you find a routine that best suits you while staying nourished and hydrated.
Despite everything I did to stay regular-ish, for a couple of stretches during my pregnancy I took a stool softener once or twice a week. That extra boost from Colace made all the difference in the world.
Always talk to your doctor or midwife first before taking any medication during pregnancy. But, if you are doing all the lifestyle things and they don’t mention a stool softener, be your own advocate and ask because they are considered safe during pregnancy.
Heartburn and pregnancy
Heartburn and reflux during pregnancy was my biggest complaint (I’m writing this at 34 weeks so hopefully that stays true).
The mechanics of reflux during pregnancy are attributed to slowed digestion catalyzed by progesterone and relaxin. The esophageal sphincters stay open longer allowing acidic food to bubble back up.
I had never experienced heartburn before. I now realize how fortunate I am to say that! It was very startling when it began.
The scariest part was waking up at night to the feeling of bringing food back up. It was not only gross and painful but made me worried about choking.
Strategies for combating heartburn during pregnancy

Changing diet: People with heartburn are often told to avoid acidic foods, spicy foods, caffeine and fried foods. With the exception of spicy foods, I honestly did not find much of a change when I avoided certain foods.
The reflux would still occur. Maybe it made it a little less painful, but certainly did not stop it from happening. I had a friend who found relief when she made dietary changes so it seems to be pretty individualized.
Avoid lying down after eating: this made a big difference for me.It was hard because I definitely enjoy curling up on the couch in the evening. But it made such a difference that I only sat upright from after dinner until bedtime.
I stopped eating two hours before bed time and tried to avoid spicy or acidic foods for dinner. I also tried not to take a nap less than two hours after eating. This was hard as a tired pregnant person!
Keeping my stomach full enough: eating a large meal was not necessarily good for reflux but an empty stomach was even worse for me. My stomach gurgles when I’m hungry and it would bring up food.
I would wake up with my stomach growling, eat some pretzels and go back to bed. Sometimes this worked and sometimes I’d be bringing up the pretzels an hour later.
I worked to find a balance, especially for dinner, so that I was full but not too full.
Typical meal schedule:
- Breakfast: 9am
- Snack: 11am
- Lunch: 1pm
- Snack: 4pm
- Dinner: 6pm
- Snack: 8pm (2-3 hours before bedtime)
This varied on the weekends when I would stay up later or certain days when I had to be up earlier. The point is that I kept my stomach full and stopped eating 2-3 hours before bedtime.
Antacids: again this article is not meant for medical advice so always talk to your provider. I reached a point where despite all the lifestyle changes, an antacid and eventually (week 33) a proton pump inhibitor (Omeprazole) was required.
Around week 15 or so, I started taking Tums a couple of times per day when I first felt the heartburn.
Then I began taking Pepcid with my prenatal vitamins at dinner. Several weeks later and after a couple of rough nights bringing up food, I asked my midwife about taking omeprazole and she gave me the green light.
Even with Omeprazole, I still occasionally needed a Pepcid in the middle of the night.
Nutrition during pregnancy
Nutrition needs during pregnancy is a huge topic which we won’t really explore here. Rather than discuss the general needs of pregnant people, I will share how I thought about food and nutrition while I was pregnant.
The most important thing to keep in mind is that you must keep yourself nourished. Now is not the time for a major change in your diet or go on a diet to lose weight.
If you are interested in individualized support, I’d be happy to work with you.
Be gentle with yourself
There is no such thing as a perfect diet, pregnant or not.
When I was too sick to eat I reminded myself that this would pass.
When I was craving ice cream or a “treat” I would have one instead of restricting myself. And guess what? The craving went away because I was satisfied.
Focus on fiber-rich foods
As we discussed above, foods rich in fiber are helpful for regularity.
Foods rich in fiber also happen to be things like vegetables, fruits, and whole grains. These foods offer a wide range of nutrients that are really important for pregnancy.
Once my morning sickness passed, I really leaned into eating those nutrient-dense foods again.
Listen to your body

It is definitely possible to have a healthy pregnancy nutrition plan as a vegan or vegetarian (although I would recommend working with a dietitian to make sure you are getting what you and baby need).
Although I was eating a primarily vegetarian-style diet before pregnancy, I ended up eating meat while pregnant because I listened to what my body was craving.
I was especially interested in eating beef and seafood. Eating animal products satisfied me and added nutrients to my diet–like iron, B12, and iodine, that I would have had to work a little bit harder to get.
Plus, a lot of plant-based proteins that I typically love like tofu, tempeh and beans, just did not appeal to me while pregnant. So, rather than force myself to follow a specific diet, I “liberalized” my diet to stay healthy.
I plan to resume my pre-pregnancy emphasis on plant-based foods when I’m ready.
Take your prenatal vitamins
I took a prenatal vitamin every day. Make sure your prenatal vitamin includes iron. The brand does not really matter.
Prenatal vitamins do not include everything you need. I recommend supplementing with:
Vitamin D: very few foods contain vitamin D naturally. And while daily time in the sun helps meet your vitamin D needs, people pregnant in the winter or with darker skin continue to be at risk for inadequate vitamin D intake.
You want at least 600 IUs of vitamin D when pregnant, but it is considered safe to take up to 4000 IU. I took 1400 IUs daily. My prenatal vitamin has 1000 IUs and my DHA supplement included 400 IU (2).
DHA: an Omega-3 fatty acid, DHA is critical for baby’s brain development. It is recommended to get at least 200 mg DHA while pregnant (3). Some prenatal vitamins contain DHA, mine did not.
I supplemented with Nordic Naturals brand Prenatal DHA which included 830 mg DHA and 400 IUs vitamin D (4).
Choline: choline is a micronutrient that supports nervous system and fetal brain development. Choline is not currently in most prenatal vitamins but it is recommended that pregnant and lactating people get 450mg/day (5).
Choline is found in a wide variety of foods, most notably meat, dairy and eggs. I supplemented with 250mg of choline daily and a varied diet that included about five eggs per week and regular consumption of meat and dairy.
A word of warning: choline is a really big molecule so the pills tend to be very large! That’s why I only took 250 mg/day. If you don’t eat any animal products, talk to your dietitian about taking more than one pill per day or finding the right regiment.
My appetite during pregnancy
I did notice an increase in my appetite during pregnancy, especially in the second trimester. I basically ate more of what I normally do– a wide variety of foods I enjoy.
There were times where I had trouble satisfying myself but this was usually because I was not eating enough fat or protein or I was searching for a flavor I was craving.
I used intuitive eating principles (see below) and nourished myself as it felt right. I did not count calories or track my food (apart from tracking fiber intake during bouts of irregularity).
Third trimester digestive issues
The third trimester did not bring any new digestive issues (at least not at the time of writing this). The most noticeable change was, unfortunately, an increase in heartburn.
I did feel some nausea as my baby got bigger and moved more–a little internal motion sickness! But it was worth it to feel him wiggling around.
Weight and body image during pregnancy

There is a constant emphasis on body weight in pregnancy. There is a “correct” amount of weight gain based on the (BS) BMI. Additionally, every pregnant person will deal with some kind of comments about their weight and the foods they are eating during pregnancy.
This can be very difficult to navigate, especially if you come into pregnancy with disordered eating or a diet culture mentality.
There is so much weight stigma from practitioners, too. It was really difficult for me because I struggle with body image issues.
I was working on healing myself from a lot of negative body image issues when I became pregnant. I was not entirely prepared with all the coping mechanisms needed to deal with this. Talking through these issues with my therapist really helped.
There is so much to say on this topic, but here are some strategies that worked for me.
Intuitive eating during pregnancy was my guiding force
If you are unfamiliar with intuitive eating, my post on plant forward nutrition and intuitive eating is a great place to start.
Intuitive eating helps you tune into your internal cues for hunger and personal health, rather than focusing on external messaging from the diet industry. This approach is designed to help you make peace with food and respect your body.
Although it was difficult at times, pregnancy changed my relationship with my body for the better. I found intuitive eating principles to be extremely useful in each trimester and stage of pregnancy.
You’ll see the 10 intuitive eating principles reflected throughout this article.
- Reject the diet mentality
- Honor your hunger
- Make peace with food
- Challenge the food police
- Discover the satisfaction factor
- Feel your fullness
- Cope with your emotions with kindness
- Respect your body
- Movement–Feel the Difference
- Honor your health–Gentle Nutrition
Don’t feel like you have to study up and be perfect at practicing intuitive eating during pregnancy. Just know that it is a tool that, with the support of a dietitian, can enrich your nutrition journey while pregnant and after!
I set boundaries with my provider about weight
You have the right to decline being weighed at the doctor’s office. Prior to becoming pregnant, I had not been weighed for years. I really had no idea how much I weighed.
Maybe I should have declined to be weighed but instead I chose a blind weight. Of course I ended up seeing my weight and my BMI on my health records and it was really difficult for me to accept that my body had changed.
I’m not sure if I would have been better off declining to be weighed (and having that conversation with every new practitioner) or weighing myself at home before I went to the doctor so I would have time to adjust.
This article on what to do about being weighed at the doctors during pregnancy was really helpful to me.
I sat with the emotional pain and worked with a therapist
I typically intellectualize problems to make them go away. And I did that to a degree (see below), but my therapist encouraged me to make space for the pain I felt.
I made space for the discomfort of acknowledging my fatphobia and all the negative thoughts I had about my body and my weight.
I learned more about weight stigma

I’ve always believed weight stigma to be real. And I’ve experienced it a little myself when my weight increased.
But when I was 32 weeks pregnant and a midwife told me to have some water before meals to “curb my appetite” I was mad as hell. I’m still mad about it while writing this.
I was, and am, in the process of learning more about being a weigh-inclusive dietitian.
Knowing that the BMI is BS and not indicative of health is not enough. So I leaned into resources like Unapologetic Eating by Alissa Rumsey, to really learn how to break free from fatphobia.
If you have any pre-existing disordered eating or body image issues, I HIGHLY recommend that you work with a weight-inclusive dietitian that can help you work through these issues. It’s painful and it’s hard but it’s worth it.
I ignored comments from family members
I have a close family member whom I have a good relationship with but always comments on my weight.
It has ruined any conversation I could ever have with her about my interests in cooking, baking, exercise and fashion because she will always bring it back to weight–either hers, mine or someone else’s.
I’d love to say that I found an insightful way to explain to her how weight is not as linked to health as we once thought and how body image and BMI is rooted in misogyny and white supremacy and not health and–most importantly address all the damage her comments have caused me.
But I didn’t. I chose to ignore her. Ultimately, I know it is her problem and not mine.
How you deal with comments from family members and friends is really up to you but I think you have 3 choices:
- Shut them down: Tell them directly that you don’t want to talk about your weight.
- Try to educate them: Explain to them how weight does not indicate health.
- Ignore them: laugh it away and/or change the subject.
Different strategies work for different people at different times.
I’m learning to respect my body
Even though it’s inevitable and natural that bodies change, it is so hard to accept. Mostly because society tells us that our bodies are best at their smallest size. This is a lie.
You don’t have to love your body now or ever, but it is important to work on how to respect it. I found this article on 8 Ways to Improve Body Image During Pregnancy to be helpful.
Digestive issues during pregnancy: final thoughts
Digestive issues during pregnancy are caused by hormonal, mechanical and dietary factors. They are uncomfortable but common.
It is important to discuss any issues with your provider to provide relief as soon as possible.
A good plan for nutrition is helpful in pregnancy to ensure mom and baby are getting their needs met.
Pregnancy can exacerbate a variety of disordered eating behaviors–often triggered by conversations with healthcare providers, unfortunately.
If you would like weight-inclusive nutrition support during pregnancy, work with a registered dietitian specializing in this type of care. I can help.